In 2016, the Joint Learning Network for UHC under the Primary Health Care (PHC) Technical Initiative brought together practitioners that formed the Health Benefits Policy (HBP) Collaborative. This collaborative consisted of experience sharing and compilation of practical advice among six low-and-middle-income countries: Indonesia, Kenya, Malaysia, Mali, Morocco, and Vietnam. Each of them conducted an assessment to evaluate their efforts in implementing new or revised benefit packages using the PHC Health Benefit Framework (HBF), a knowledge product that was developed from the collaborative. 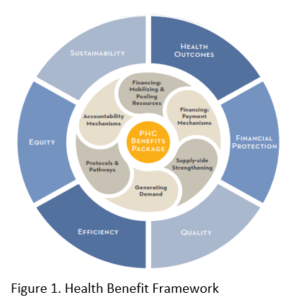
Kenya participated by sharing experience from a sub-national level, namely Makueni County, which is one of the 47 sub-national governments of the country. Makueni County established the MakueniCare UHC Programme in 2016 with an effort to provide coverage for the county residents. To access the programme, the registration fee per household was Ksh 1000 (USD 8.60) annually to cover the principal, spouse and five dependents below 18 years of age. The members can access services at level 5 and 4 county health facilities. The programme runs complementary to other health programs such as the program for free PHC implemented by the national government and the National Health Insurance Fund (NHIF), which is to be accessed as a last resort. The benefit package consists of the extent of the services available at the county health facilities and services covered/not covered in the complementary programmes. The services include inpatient, outpatient, and mortuary service with exemption of auxiliary devices and cost of surgical implants; forensic services; specialized services e.g., CT scanning, surgical implants, intensive care unit services, dialysis, non-routines medical reports, professional fees for autopsies/postmortems, medical reports and other related services, and referrals to outside the County.
Five years later in 2022, the JLN Kenya Country Core Group (CCG) with support from JICA and working with Makueni County Department for Health in the course of 3 months used the HBF to assess MakueniCare Programme, to check on the progress towards providing UHC to the residents of the County, and to inform the Kenya country JLN chapter on key areas on which to focus as the team plans to launch a sub-national JLN chapter. See the table below for the outcomes of the programme assessment based on the six policy domains from the HBF:
| Policy Domain | Domain Definition | Findings |
|---|---|---|
| Financing: Mobilizing and Pooling Resources | The strategy for pooling resources that finance service delivery. | Sources of health financing:
|
| Financing: Payment Mechanisms | Provider payment mechanisms set up to incentivize providers to offer package services. |
|
| Supply Side Strengthening | Government’s spending to improve provider capacity to deliver prioritized PHC services. |
|
| Generating Demand | The health system steward’s strategy for educating the public about services within the package and beneficiary enrollment. |
|
| Protocols and Pathways | The treatment protocols and referral pathways that are put in place to improve quality and efficiency of service delivery. |
|
| Accountability Mechanisms | The regulatory framework for monitoring and evaluation systems that accompany the PHC benefits package |
|
The assessment noted significant positive impact on the side of the policy objectives that drive a responsive PHC-oriented reform ass identified in the HBF – health outcomes, financial protection, quality, efficiency, equity, and sustainability. However, some areas still required investment and effort to improve the programme’s delivery as outlined in the recommendations below.
- Costing of the devolved county health services so that health funding is evidence based as opposed to blind allocation of resources.
- Establishing performance-based financing to encourage all facilities to increase their share revenue from the different sources such as NHIF capitation, rebates, inpatient reimbursement and have targets captured in performance contracts for facility heads. This goes a long way in increasing the health funding for facilities hance better service delivery.
- Developing and strengthening innovative healthcare financing for communities’ by periodically reviewing the criteria for resource allocation and purchasing mechanisms to improve efficiency and utilization of resources;
- Enhance prepayment mechanisms towards UHC. The introduction of the 14 days waiting period is positive but proposals from Health Administrators to increase the period will help with better planning based on the resources collected for UHC registration that contributes to the hospital funds retained by the facilities budgeted quarterly.
- Promoting private sector participation in financing of healthcare through public private partnerships and other mechanisms.
- Automation- involve the user department and also enhance access by hosting the servers at the health department for ease of access and efficient service delivery.
- Developing and implementing a health information systems (HIS) policy; Facilitating access to information to the public while protecting privacy and confidentiality.
The MakueniCare assessment led to many lessons learned that can be used by other counties, the Kenyan government, and even other low- and middle-income countries looking at implementing responsive PHC-oriented reform, in areas such as making a case for healthcare funding, ring-fencing and retaining health revenues by health facilities, health investment to improve access and quality of care, performance-based budgeting, legislation, governance and public participation. With this assessment, Makueni County can chart the way in addressing challenges while leveraging on its strengths on the journey to ensuring UHC for all in the county. With the resources available from JLN and other partners, this is possible.
Special thanks to JICA for the financial support and JLN for the technical support