Advancing Universal Health Coverage in Malaysia: Harmonizing Country Priorities with Collaborative Learning
Authors:Dinash Aravind, Premila Devi Jeganathan, Khor Shu Lin, Mohamad Azim Mohd Azmi, Isha Sharma, Jane Nyambura, Rahul S Reddy Kadarpeta
As countries progress towards UHC, it’s crucial to understand that the goalposts are dynamic. UHC represents not just a destination, but a continuous journey aimed at enhancing health system performance to achieve equitable population health and ensure financial risk protection¹ . It is essential to contextualize global learnings on UHC and make them relevant to enhance the capabilities of in-country stakeholders, especially policymakers, technical leaders, and practitioners. This enables them to appreciate the diversity of their country’s local health systems, identify problems, and address them with context-specific solutions. It is crucial to tailor reforms as health systems evolve dynamically.
JLN operates on this premise, and in this blog, we share JLN’s contributions towards strengthening Malaysia’s capacities to progress towards UHC. JLN adopts a country-driven and joint learning approach that engages practitioners in learning from each other to address challenges as well as co-produce practical solutions for implementing UHC reforms. In this process, JLN prioritizes the specific needs of each country articulated in member countries’ policies and initiatives, when planning its technical offerings. Additionally, they are voiced in the JLN’s annual Country Core Group Survey, administered to each member country. These standardized and consistent institutional practices have enabled JLN to expand its membership from 6 countries in 2009 to 39 in 2024, remaining relevant in addressing emerging challenges through technical initiatives such as health emergency preparedness, digital health, contracting of health services, and primary healthcare performance management.
Malaysia has been consistent on its pathway towards UHC. Health has always remained an important agenda of the government with it being an essential and integral part of Malaysia’s government policies. Over the years to address the need of the population, Malaysia has embarked on many initiatives to improve UHC through sharing of resources within an integrated network of hospitals, bringing healthcare closer to the community such as mobile clinics, ambulatory services, domiciliary care, rural low risk birthing centres, innovative value-added medicine supply services and various other initiatives².
Among the Western Pacific region countries, Malaysia has improved its UHC service coverage index from 52 in 2000 to 76 in 2021. Malaysia is unique in the sense that while Out-of-Pocket (OOP) expenditure averages around 35%, the incidence of catastrophic health expenditures remains relatively low at 1.5%³.
Nevertheless, Malaysia faces various health issues and challenges such as aging population, increasing double disease burden, inflation of health care cost and high demand for quality services¹.
In the 12th Malaysia Plan, health and healthcare was a priority area under the theme Strengthening Security, Wellbeing, and Inclusivity. Some of the key targets emphasized on were redesigning service delivery and improving access, strengthening health financing to be on a sustainable footing, improving health literacy, enhancing public-private partnerships, and leveraging on digital technologies.
In 2016, Malaysia embarked on a journey towards innovative health financing mechanisms via the establishment of ProtectHealth Corporation Sdn. Bhd. (PHCorp), a non-profit government owned company under the Ministry of Health (MOH) to improve access and enhance the effectiveness of the healthcare system while ensuring reasonable healthcare costs. PHCorp is a not-for-profit company incorporated to coordinate, administer, and manage initiatives related to financing healthcare services as mandated by MOH.
As a strategic purchaser, PHCorp is the implementer for several MOH initiatives such as Skim Peduli Kesihatan for the B40 group (PeKa B40), Skim Perubatan MADANI as well as the coordinator for the National COVID-19 Immunisation Programme (PICK) via collaboration with private general practitioners. PeKa B40 scheme is designed to increase screening uptake for non-communicable diseases (NCDs) among Malaysians aged 40 and above, with a focus on the lower-income group, specifically the lower 40% income group. Skim Perubatan MADANI is a programme that contracts private health clinics to provide acute care access for the targeted population. Throughout these programmes, ProtectHealth innovates to develop a new payment mechanism dashboard and improves on its role as strategic purchaser when contracting providers to enable the delivery of efficient and good quality healthcare services. Besides PeKa B40 and Skim Perubatan MADANI, the Ministry of Finance (MOF) provides additional financial assistance for medical treatment via an initiative known as mySalam B40 Takaful Protection Scheme. This scheme offers basic protection that includes hospitalization and critical illness benefits.
Further, in 2023, Malaysia’s parliament passed the Health White Paper (HWP) For Malaysia which puts forth a holistic document for systemic and structural reforms of the Malaysian health system. The HWP responds to the nation’s health challenges and aims to ensure greater equitability, sustainability, and resilience of the health system. These reforms spanning over 15 years are based on four major pillars:
- Transforming Health Service Delivery
- Advancing Health Promotion and Disease Prevention
- Ensuring Sustainable and Equitable Health Financing
- Strengthening the Health System’s Foundations and Governance.
As an initial step to move the reform, the Ministry of Health has established a Health Transformation Office (HTO). HTO is entrusted with leading the comprehensive transformation of Malaysia’s health system, aligning with the aspirations outlined in the HWP.
The country aspires to achieve these milestones and has encouraged commitment from all stakeholders to learn, translate and adapt learnings from country experiences in the region and globally. For example, as a JLN member country actively participating since 2010, Malaysia has facilitated access for its policymakers and technical leaders to global knowledge on health systems strengthening and reform. With expert facilitation, the JLN employs a collective problem-solving approach that draws on experiences from multiple countries in a structured manner. This approach helps frame problems, identify common issues, explore insights and knowledge, and synthesize practical solutions that are tailored to each country while being globally adaptable. These insights derive from peers’ tacit knowledge, answering questions like “What has worked?” and “What has not?”, and provide steps to achieve program objectives. Malaysia has benefited from this process and co-developed several Knowledge Products (KPs) presented in Figure 1.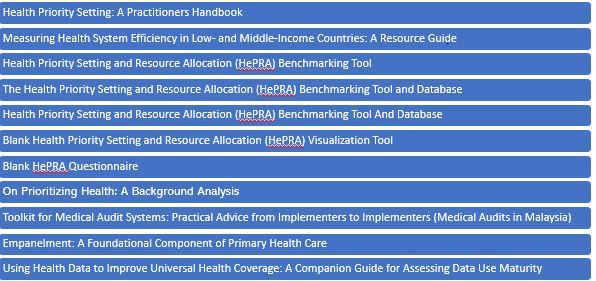
Malaysia has effectively adapted and implemented, two of these KPs. The UHC Primary Health Care Self-Assessment Tool (UHC-PHC Self-Assessment Tool), provided a structured approach to identify practical policy opportunities for improving the relationship between health financing and primary health care (PHC) strengthening efforts within the existing system. As an impact, the adaptation of the tool created the evidence base which helped to evaluate and improve the public-private partnership challenges at the national policy level. It also enabled a platform for collaboration between policymakers, government officials and private providers which contributed to MOH Malaysia’s strategic plan 2016-2020 focused on increasing access to PHC services.
The Toolkit to Develop and Strengthen Medical Audit Systems detailed how to set up medical audit units and conduct step-by-step claims reviews, as practical guidance for practitioners. This contributed greatly to the establishment of an independent Medical Audit Section in Malaysia managed by ProtectHealth Corporation (PHCorp). This section regularly reviews more than 2000 PeKa B40 claims per month. The quality of healthcare services provided by both public and private healthcare providers can be evaluated, subsequently this allows for quality improvement recommendations from PHCorp. For example, many cases, including cases of misdiagnosis and incomplete lab or medical histories, have been identified5. PHCorp as implementer of National COVID-19 Immunization Programme by Private Medical Practitioners also utilized the audit function to evaluate the quality and compliance of the appointed practitioners.
Malaysia also participated in JLN’s country pairing learning exchange with Ghana and Philippines to address specific challenges. During this virtual exchange, Ghana and the Philippines shared insights on their experiences in developing and operationalizing mechanisms for provider monitoring, including the evolution and lessons learned from Medical Audit (MA) practices, particularly within primary and tertiary healthcare services. The focus was mainly on treatment and diagnostics for chronic non-communicable diseases (NCDs) and methods for incentivizing or penalizing providers. The learning exchange was enlightening and fostered a rich environment for sharing best practices and innovative approaches to boost the healthcare quality.
These exemplary efforts demonstrate Malaysia’s commitment to responding to the changing health systems context and augment its performance through shared knowledge and innovation. The World Health Organization (WHO) continues to acknowledge Malaysia as providing quality healthcare services based on its high-performing health system and well-trained workforce6 Malaysia’s commitment to achieving Universal Health Coverage (UHC) has positioned the country as a model in Southeast Asia and JLN’s contribution to support Malaysia’s emerging needs will continue to build a resilient and inclusive healthcare system that serves all its citizens effectively. Learn more about JLN’s technical offerings operational in 2024 here.
About the Authors: Dinash Arvind is Senior Assistant Director , Health Transformation Office, MoH, Malaysia, Premila Devi Jeganathan is Deputy Director, Dr. Khor, Chief Assistant Director and Dr Mohamad Azim bin Mohd Azmi, Chief Assistant Director at National Health Financing Section, Planning Division, MoH Malaysia; Isha Sharma is Program Officer JLN, Jane Nyambura is Program Officer, JLN and Rahul Kadarpeta is Executive Director JLN.
Reference
- Kutzin J. Health financing for universal coverage and health system performance: concepts and implications for policy. Bull World Health Organ. 2013 Aug 1;91(8):602-11. doi: 10.2471/BLT.12.113985. Epub 2013 Jun 17. PMID: 23940408; PMCID: PMC3738310.
- Strengthening Health Systems and Access to Care – Best Practices in ASEAN Jakarta: ASEAN Secretariat, December 2019
- World health statistics 2023: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2023
- Healthcare Asia Magazine. (2024). Malaysia’s ageing population to drive healthcare demand. Healthcare Asia Magazine. https://healthcareasiamagazine.com/healthcare/news/malaysias-ageing-population-drive-healthcare-demand
- Joint Learning Network for Universal Health Coverage. (2021). Medical audits in Malaysia.https://jointlearningnetwork.org/wp-content/uploads/2021/01/FINAL-Medical-Audits-in-Malaysia.pdf
- Lo, YRJ. and Allotey, P. World Health Day 2018. Lesson from Malaysia on Universal Health Coverage, World Health Organization.